Understanding Pulmonary Hypertension and Its Impact on Premature Infants
In recent years, fresh evidence has emerged that connects pulmonary hypertension, the use of inhaled nitric oxide (iNO), and the onset of retinopathy of prematurity (ROP) in preterm babies. As a long-term observer of neonatal care, I find this topic rich with both promise and caution. The study we’re discussing today digs into the countless twists and turns of neonatal care, prompting us to re-examine how we manage treatment strategies in extremely fragile patients.
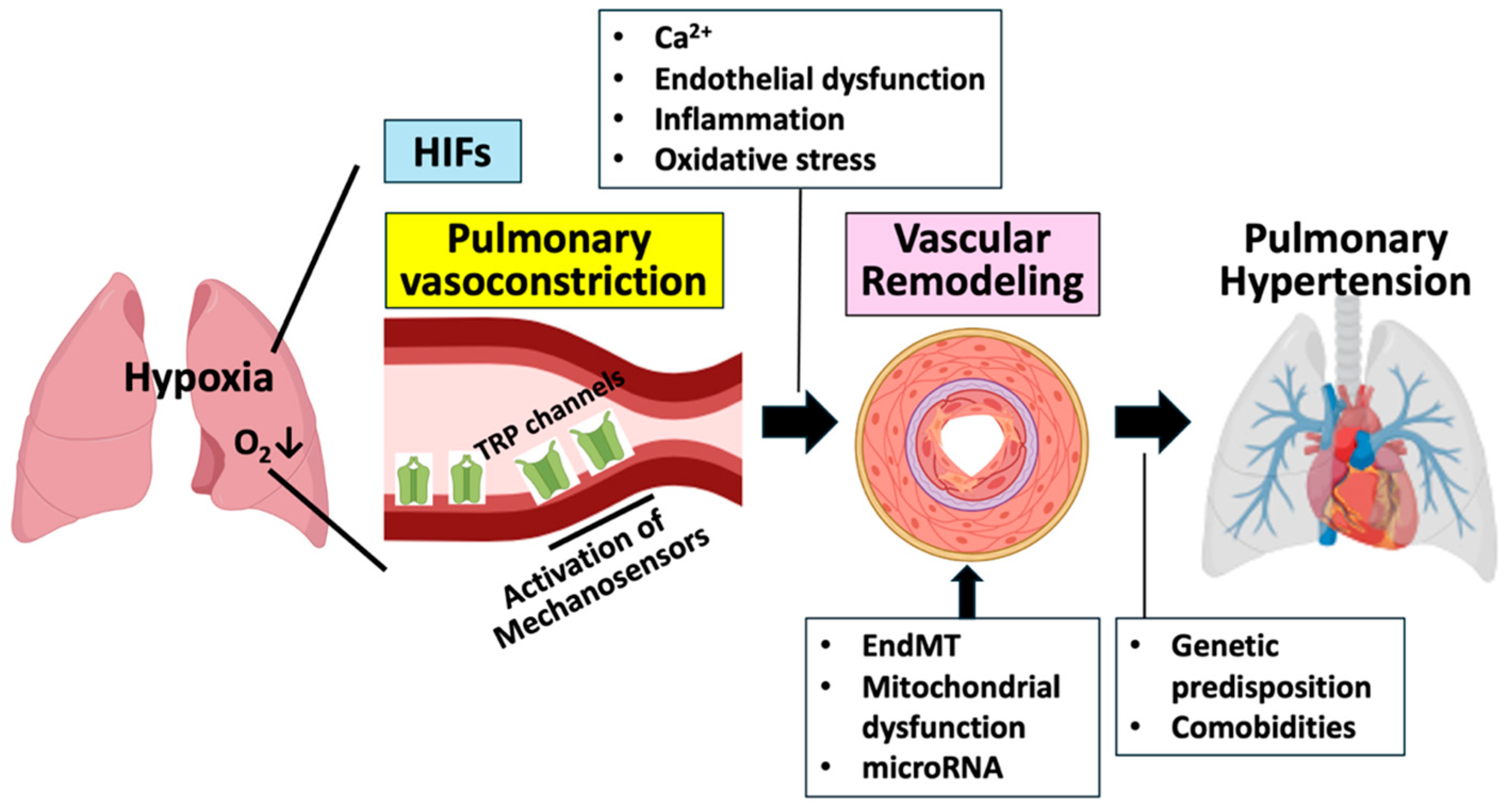
Premature infants are, by nature, vulnerable—especially when it comes to respiratory and vascular issues. Pulmonary hypertension, which is marked by increased pressure in the lungs’ arteries, poses a serious risk for these infants due to their underdeveloped lung structure. The tricky parts of managing this condition are compounded by the need for effective therapies that improve oxygenation without leading to further complications.
Given these conflicting demands, the use of inhaled nitric oxide (iNO) has become common practice in many neonatal intensive care units (NICUs). iNO is a selective pulmonary vasodilator, meaning it helps open up blood vessels in the lungs and boosts oxygen levels. The challenge, however, lies in understanding how this treatment might affect other developing organ systems, such as the eye, where abnormal blood vessel growth can lead to ROP.
The Tricky Parts of Pulmonary Hypertension Treatment in Newborns
Pulmonary hypertension treatment in preterm infants is full of tangled issues. The complications arise from the fact that premature lungs are not fully formed and are still adapting to the extra-uterine environment. In many cases, the blood vessels in the lung are not yet able to control the resistance needed for proper blood flow. The following list helps to clarify some key challenges:
- Underdeveloped lung tissue leading to chronic oxygen deprivation
- Inconsistent responses to therapies due to variations in lung maturity
- Balancing oxygen supplementation with the risk of oxygen toxicity
- Managing complications that include both immediate respiratory issues and later systemic effects
Each of these points represents a confusing bit in the overall puzzle of neonatal care. Medical professionals must consistently figure a path through these complication-laden scenarios, aiming to provide the most effective yet safe treatment options for their littlest patients.
Inhaled Nitric Oxide: A Double-Edged Sword?
Inhaled nitric oxide has been a cornerstone in treating pulmonary hypertension among preterm infants because it directly benefits the compromised pulmonary vasculature. By selectively dilating the lung’s blood vessels, iNO helps improve oxygen delivery and reduce the workload on the right side of the heart. However, its role is not without controversial twists and turns.
Critically, while iNO offers an immediate pulmonary benefit, emerging evidence suggests that the dosage, timing, and duration of iNO exposure may also influence other areas of a premature infant’s development. In particular, the effect on retinal vascular development has garnered attention, as ROP remains one of the most significant sight-threatening conditions in this population.
This dual nature of iNO raises a classic clinical dilemma: how to harness its benefits for respiratory support while avoiding potential unwanted side effects in other organs? The answer requires a balanced approach that considers both the pulmonary benefits and the retinal risks involved.
How Nitric Oxide Influences Retinal Vascular Development
The eye, especially the retina, is delicate in premature infants. The development of the fragile retinal blood vessels is easily disturbed by factors such as oxygen levels and growth factors. If these vessels grow abnormally, they can lead to a condition known as retinopathy of prematurity (ROP), a disorder that may cause permanent visual impairment if not managed properly.
Recent research, drawing from extensive datasets pulled from the U.S. national health database, indicates that there might be a notable association between the use of inhaled nitric oxide and the frequency and severity of ROP in preterm infants. This long-overlooked connection invites us to look into the nitty-gritty of how iNO might modulate retinal blood vessel formation.
From a scientific standpoint, the mechanisms at work involve the interplay between nitric oxide’s role as a vasodilator and its influence on vascular endothelial growth factor (VEGF) pathways—key regulators of angiogenesis. When these pathways are disrupted, the careful balance of retinal blood vessel growth can tip towards abnormal proliferation, leading to ROP. It is a fine balance characterized by subtle details and small distinctions between beneficial and potentially harmful outcomes.
Linking Pulmonary Issues and Retinal Health: Evidence from U.S. Data
A recent study makes it clear that there is a tangled web connecting pulmonary hypertension in preterm infants, the administration of iNO, and the heightened risk of developing severe ROP. When clinicians look at outcomes from a U.S.-wide dataset of neonatal care, they find that the infants treated with inhaled nitric oxide display a shift in the risk profile for ROP, especially when considering the timing and amount of nitric oxide they received.
Using advanced statistical methods and controlling for several factors—such as gestational age, birth weight, oxygen supplementation duration, and concurrent health conditions—the researchers provided robust evidence of this relationship. Their multivariable regression models helped isolate the independent risk of ROP, offering valuable insight into how the severity of pulmonary hypertension might modulate retinal outcomes.
This kind of comprehensive analysis helps sort out the tricky parts of neonatal care. It reveals a layered picture: iNO might be essential for maintaining pulmonary function, yet its systemic effects can also put the retina at risk. It is a challenging balancing act that medical professionals must grapple with on a daily basis in the NICU.
The Fine Points of Retinopathy of Prematurity (ROP) in Neonatal Care
ROP is a condition defined by abnormal growth of blood vessels in the retina. This abnormal vascular proliferation can lead to retinal detachment and, ultimately, vision loss. The delicate intricacies of this condition are loaded with problems and subtle issues that demand careful monitoring and intervention.
Here are some key factors that contribute to the onset and progression of ROP:
| Factor | Impact on ROP |
|---|---|
| Oxygen Levels | High supplemental oxygen can cause blood vessels to constrict and then proliferate abnormally during recovery. |
| Gestational Age | Lower gestational age is strongly associated with a higher risk due to less developed retinal vasculature. |
| Birth Weight | Smaller infants often face greater challenges in developing healthy retinal blood vessels. |
| Inflammatory Factors | Systemic inflammation in preterm infants may further disrupt the normal process of retinal vessel development. |
Understanding these details is critical. It is the little twists and turns—such as slight fluctuations in oxygen saturation or minor changes in dosing—that can dramatically influence the final outcome for these newborns. Hence, clinicians are encouraged to take a close look at each element contributing to the risk of ROP, while also considering the pulmonary benefits provided by treatments like iNO.
Considering the Clinical Implications: Balancing Benefits and Risks
For everyday neonatal care, the findings discussed prompt a serious rethinking of how we use inhaled nitric oxide. On one side, iNO provides an effective, sometimes life-saving, method to get around the tricky parts of pulmonary hypertension. On the other side, there is mounting evidence that its use is linked to the development of vision problems down the line—particularly ROP.
This balancing act is not just an academic discussion; it carries heavy real-world consequences. Neonatologists must now consider whether to adjust their current protocols for iNO use, especially regarding its dosage, timing, and duration. The objective is to optimize therapeutic benefits while avoiding potentially overwhelming adverse outcomes in retinal development.
Some key clinical considerations include:
- Vigilant screening and regular ophthalmologic evaluation for infants receiving iNO.
- Personalized treatment plans that factor in an infant’s gestational age, birth weight, and overall health status.
- The possibility of exploring alternative pulmonary treatments that might offer safer profiles for retinal health.
- Continuous review of existing neonatal care protocols in light of new evidence, weighing pulmonary benefits against potential systemic risks.
These points underline the importance of collaboration among neonatologists, pulmonologists, and ophthalmologists. By working together, these experts can navigate the confusing bits of neonatal care, striving to strike the right balance between respiratory support and safeguarding vision.
Optimizing Therapeutic Regimens in the NICU: Finding Your Path Through Treatment Options
Given the complexity and the high stakes involved, a one-size-fits-all strategy is simply not enough. Instead, a more personalized medicine approach is gaining traction. Such an approach considers each infant’s unique combination of health challenges and genetic predispositions, ensuring that treatment regimens are as carefully tailored as possible.
Advances in medical technology now allow for better monitoring not just of pulmonary status but also of retinal health. Continuous oxygen monitoring, better imaging devices for the retina, and improved data analysis techniques help caregivers figure a path that minimizes potential adverse effects. When these measures are combined with individualized dosing strategies for iNO, the potential for a positive overall outcome increases significantly.
A few strategies that have been proposed include:
- Customized Dosing Protocols: Adjusting iNO doses based on specific outcome predictors such as oxygen saturation levels and indicators of retinal stress.
- Early Screening Tools: Implementing more frequent eye exams to quickly identify signs of ROP before they progress to severe stages.
- Alternative Therapeutic Agents: Considering other pulmonary vasodilators which might offer similar benefits with fewer systemic side effects.
- Multi-disciplinary Care Teams: Bringing together experts from different fields to manage care, ensuring that perplexing bits of treatment decisions are shared and discussed from all angles.
These strategies are geared toward designing a safer, more effective means of managing neonatal pulmonary hypertension while also protecting the delicate process of retinal development.
Future Research Directions and Policy Implications
While current data from large databases provides compelling evidence of a link between iNO therapy and ROP, there remains a strong need for further research. Prospective, randomized trials will be crucial to help confirm these observational findings and to explore the underlying biological mechanisms at play.
Some areas ripe for future investigation include:
- Studying alternative dosing regimens and exposure durations for iNO to pinpoint a protocol that minimizes retinal risks.
- Exploring new pulmonary vasodilators that might offer similar respiratory benefits without adversely affecting retinal development.
- Investigating genetic markers that could predict which infants are more likely to develop ROP in response to standard treatments.
- Developing advanced monitoring techniques to detect early changes in retinal vascular growth patterns in preterm infants.
Policy makers in the healthcare field must take these emerging insights into account when crafting or updating clinical guidelines. By doing so, they can help ensure that the standard of care in NICUs not only supports immediate respiratory stability but also safeguards long-term visual outcomes for these vulnerable patients. The policy changes might include revising risk stratification criteria to incorporate factors like PH severity and iNO dosing parameters, as well as recommending more frequent and systematic eye examinations for those receiving therapy.
Interdisciplinary Collaboration: Tackling the Tangled Issues Together
As we continue to untangle the confusing bits of neonatal care, one clear message stands out: no single discipline can manage all aspects of this challenge alone. Neonatologists, pulmonologists, and ophthalmologists must work side by side to dissect the intertwined effects of therapies like iNO. Such collaboration not only enhances understanding but also leads to more holistic treatment plans tailored to the unique needs of premature infants.
Interdisciplinary collaboration enables the following benefits:
| Benefit | Description |
|---|---|
| Comprehensive Monitoring | Combining expertise from different specialties allows for both respiratory and ocular systems to be monitored closely. |
| Individualized Care | Teams can consolidate insights from various fields to craft a personalized treatment plan that addresses both immediate and long-term needs. |
| Enhanced Research | Collaboration fosters a multidisciplinary research environment that is more likely to identify subtle issues and develop innovative solutions. |
| Policy Updates | Gathered expertise from several specialties can better inform policy makers, leading to improved guidelines and standard practices. |
This cooperative approach is key to steering through the complicated pieces of neonatal care, ensuring that both pulmonary function and visual outcomes are optimized.
Conclusion: Balancing Pulmonary Benefits with Retinal Safety in Neonatal Care
In summary, recent evidence drawn from the U.S. national database is prompting a much-needed re-evaluation of inhaled nitric oxide use in newborns with pulmonary hypertension. While iNO offers essential support to the fragile respiratory systems of preterm infants, its potential side effects on retinal vascular development call for cautious and nuanced application.
The data reveals that the relationship between iNO therapy and retinopathy of prematurity is by no means straightforward. Instead, it is characterized by several subtle details and small distinctions that impact both short-term respiratory outcomes and long-term visual health. This dual nature is full of problems that require us to figure a path between life-saving therapy and minimizing unintended complications.
As clinicians work through the tangled issues of neonatal care, the take-home message is clear: careful dosing, vigilant monitoring, and personalized treatment approaches are super important. It is imperative to set up multifaceted monitoring systems that not only track pulmonary outcomes but also keep a close eye on retinal development.
Future research, including well-designed prospective trials, will be pivotal in clarifying the best practices for using iNO in this setting. In the meantime, policy makers and healthcare providers must remain flexible, adapting current protocols based on emerging evidence. Interdisciplinary collaboration will serve as the cornerstone of these efforts, ensuring that every aspect of a preterm infant’s care is managed with a balanced perspective.
Ultimately, our goal remains to support the survival of these vulnerable infants while also prioritizing their quality of life in the long run. By embracing the dual responsibility of optimizing both pulmonary and ocular outcomes, the neonatal care community can move toward a future where every infant has a better chance for both a healthy start and a bright visual future.
Originally Post From https://bioengineer.org/pulmonary-hypertension-nitric-oxide-and-premature-retinopathy/
Read more about this topic at
Factors Influencing Receipt and Type of Therapy Services …
A Collaborative Approach to Defining Neonatal Therapy