Gene Therapy Innovations and Modified AAV Variants
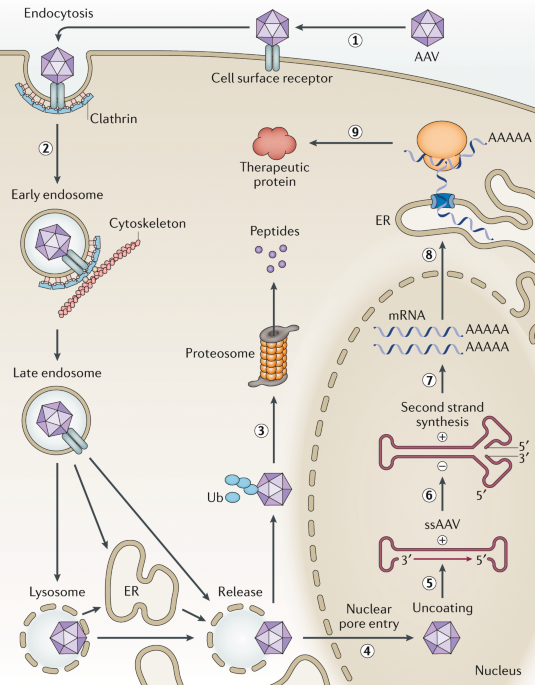
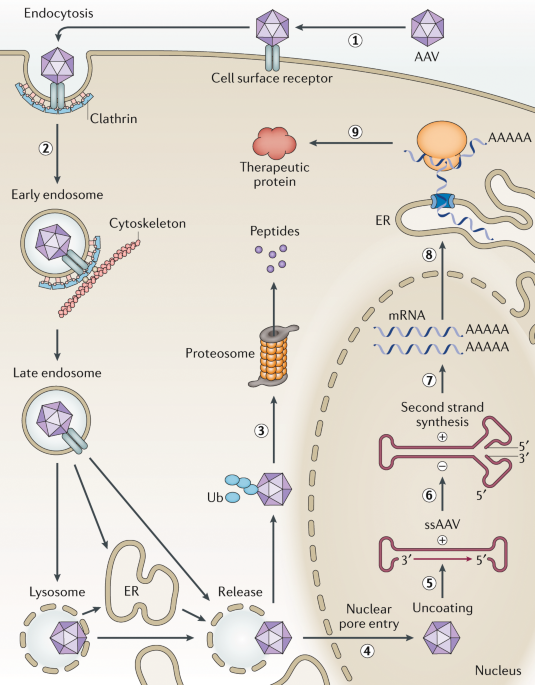
The field of gene therapy has seen a surge of promising innovations in recent years, and one area gaining increasing attention is the study of modified adeno-associated virus (AAV) variants. These viral vectors, long used to deliver therapeutic genes, have been re-engineered to address the tricky parts of gene delivery—particularly the challenge of achieving efficient transduction in human vascular endothelial cells. This new approach is not only critical for cardiovascular treatments but also represents a key leap forward in treating various genetic disorders with a targeted, cell-specific strategy.
A recent investigation, published in a notable peer-reviewed journal, showcases how modifications to AAV vectors can improve the delivery of genetic material where it matters most. The study, guided by the work of Stamataki and colleagues, focuses on redesigning the viral architecture to overcome the tangled issues that often hinder effective gene therapy. Throughout, the researchers highlight the necessity of refining these delivery systems to better reach vascular endothelial cells, which are a central component of blood vessel function and overall cardiovascular health.
Gene therapy, by its nature, must contend with a series of complicated pieces—from recognizing the target cells to managing the body’s immune response. The attractiveness of using modified AAV variants lies in their potential to address these hidden complexities while still achieving robust and sustained therapeutic effects. In these pages, we will take a closer look at how these advancements promise to improve outcomes, the methods used to engineer these vectors, and their implications for clinical therapies.
Enhancing Transduction Efficiency in Vascular Cells
One of the most nerve-racking challenges in gene therapy has been to ensure that the vector can effectively “get into” the desired cells. Human vascular endothelial cells, which line the interior surfaces of blood vessels, play a critical role in regulating blood flow, immune function, and even wound healing. The modifications made to AAV variants aim to tackle the confusing bits and twists and turns associated with vector entry and gene transduction.
Targeting the Fine Points of Cell Interaction
At the heart of the research is an exploration into the subtle parts of how viral particles interact with cell membranes. Traditional AAV vectors, while safe, have historically been limited by their suboptimal engagement with the vascular cell surface. The newly engineered variants incorporate adjustments that allow for better attachment and penetration into the cell’s interior, ensuring that the therapeutic genes can be delivered more reliably.
Some of the key alterations include:
- Changes in the capsid proteins to improve binding affinity
- Structural modifications to bypass cellular barriers
- Adjustments aimed at evading the immune system’s detection
These improvements are designed to address the tiny details—those subtle differences in receptor engagement and intracellular trafficking that can mean the difference between success and failure in gene therapy applications.
Improving Gene Delivery Mechanisms
One of the trickiest aspects of modifying viral vectors is ensuring that they can safely and efficiently ferry genetic material without causing unintended side effects. The modifications in the AAV variants allow for a more focused and sustained delivery of target genes into the vascular endothelial cells. In this way, the engineered vectors can help overcome many of the traditional barriers to transduction efficiency in therapeutic applications.
A schematic overview of the improvement process might look like this:
| Process Step | Traditional AAV | Modified AAV Variant |
|---|---|---|
| Cell Attachment | Limited receptor binding | Enhanced receptor recognition |
| Endocytosis | Inefficient internalization | Optimized internalization pathways |
| Nuclear Delivery | Suboptimal gene release | Sustained gene expression |
This table outlines some of the little twists that researchers have been addressing, demonstrating a clear path toward better transduction efficiency in targeted cells.
Refining Viral Vectors for Human Vascular Endothelial Cells
The emphasis on human vascular endothelial cells is not accidental. These cells are crucial for maintaining the health of the cardiovascular system, influencing blood pressure, clotting mechanisms, and even inflammatory responses. By focusing on these key cellular players, the modified AAV variants show promise not only for genetic diseases but also for conditions such as atherosclerosis, hypertension, and even certain forms of heart failure.
Engineering Details and Methodological Approaches
To achieve improved gene delivery outcomes, researchers have taken a closer look at the nitty-gritty of AAV vector design. One approach has been to fine-tune the viral capsid structure, which is the outer protein shell of the virus responsible for binding to and entering cells.
Some of the methods employed include:
- Site-Directed Mutagenesis: This technique allows scientists to make precise changes to the viral capsid, enhancing its ability to bind to receptors on vascular cells.
- Peptide Display Libraries: By screening different peptides on the viral surface, researchers can identify sequences that improve cell targeting.
- Directed Evolution: This method involves iterative rounds of mutation and selection, ultimately leading to variants with superior transduction capabilities.
Each of these technical approaches helps to dig into the fine details of gene therapy, ensuring that the modifications are both effective and safe. Although the process of optimizing these vectors might feel like sorting out a maze of interconnected issues, the emerging results are clear—more efficient gene delivery systems can be designed with careful, systematic modifications.
Balancing Safety with Efficacy
A critical aspect of developing any gene therapy vector is achieving the right balance between safety and efficacy. Modified AAV variants are celebrated not only for their improved targeting but also for their commendable safety profile. Historically, AAV-based vectors have enjoyed a reputation for mild immune responses and minimized risks of insertional mutagenesis. By enhancing the design, researchers are making the overall system even more robust, reducing potential side effects while ensuring robust gene expression within the target cells.
The following points highlight the key benefits of these modifications:
- Enhanced Specificity: Improved binding to vascular endothelial cells minimizes off-target effects.
- Reduced Immune Activation: Fine-tuned surface proteins help the vector avoid triggering aggressive immune responses.
- Sustained Gene Expression: The improved vector design allows for long-term maintenance of therapeutic gene expression, which is essential for chronic conditions.
- Versatility: These vectors have the potential to be adapted for a range of different gene therapy applications.
Overcoming the Tricky Parts of Gene Therapy Delivery
The journey from laboratory research to the transformation of clinical therapies can appear intimidating and riddled with challenges. Researchers must figure a path through a series of confusing bits and tangled issues inherent in viral vector design and application. Some of these challenges include immune system responses, optimal dosing regimens, and even the manufacturing of consistent viral batches with high purity and potency.
Addressing Immune System Barriers
One of the classic hurdles in gene therapy is the body’s immune response to viral vectors. Even modified AAVs, despite their well-known safety profile, can provoke immune reactions that may limit their effectiveness. The novel modifications described in recent studies aim to reduce these responses by altering antigenic sites on the viral capsid, making it more difficult for the body to recognize and attack the vector.
Consider these steps to mitigate immune activation:
- Capsid Shielding: Masking specific antigens to remain less visible to the immune system.
- Transient Immunosuppression: Employing mild, temporary immunosuppressive drugs during the vector’s administration.
- Dose Optimization: Finding the ideal balance between therapeutic efficacy and minimal immune activation.
These strategies not only address the immediate challenges but also provide a roadmap for future adjustments in vector design. By carefully steering through these obstacles, researchers continue to transform what once were overwhelming challenges into manageable steps along the path to clinical application.
Optimizing Dosing Strategies
Another confusing bit in gene therapy is the determination of the correct dosing regimen. Too low a dose may result in insufficient therapeutic gene expression; too high might cause unintended toxicities or immune responses. The modified AAV variants have been tested using a range of doses in preclinical studies, revealing a sweet spot where gene delivery is both safe and effective.
A simplified overview of the dosing considerations includes:
- Low Dose: Might not achieve the required level of gene expression to be effective.
- Medium Dose: Helps achieve effective therapeutic levels while keeping the immune response in check.
- High Dose: Could overwhelm cellular processes or trigger off-target effects.
Researchers need to get into the details of each dosing level to ensure that the modified vectors perform optimally. By taking a closer look at these dosing challenges, it becomes clear that careful titration is essential for maximizing benefits while minimizing risks.
Practical Implications for Cardiovascular and Beyond
The promise of these innovative modified AAV variants is not limited to rare genetic disorders; it extends broadly to cardiovascular health and other therapeutic areas. The success of targeted gene delivery into vascular endothelial cells opens up several practical avenues for treatment development.
Targeted Treatments for Cardiovascular Diseases
Cardiovascular diseases remain a major health challenge worldwide. By directing therapeutic genes specifically to vascular endothelial cells, the modified AAV vectors have the potential to treat conditions such as:
- Atherosclerosis: By improving endothelial function, gene therapy could reduce plaque buildup in arteries.
- Hypertension: Targeting blood vessel cells might result in better regulation of blood pressure.
- Ischemic Heart Disease: Enhanced gene delivery could contribute to improved blood flow and reduced damage following cardiac events.
These targeted approaches demonstrate how precision medicine, powered by advanced gene therapy techniques, can offer more personalized and effective treatment options. While the road from preclinical success to clinical application is long and filled with nerve-wracking twists, the potential rewards are enormous.
Expanding Horizons: Beyond Cardiovascular Therapies
Though cardiovascular applications are among the most promising, the improved gene delivery methods have implications for other fields as well. Chronic conditions that involve other types of endothelial dysfunction, including certain neurological disorders or inflammatory diseases, might eventually benefit from these refined AAV variants. Their versatility further underlines a broader trend towards the development of therapies that are both highly specific and broadly applicable.
For example, the possibility exists for applying similar strategies in the treatment of:
- Neurovascular Disorders: Where the integrity and function of blood vessels in the brain are compromised.
- Diabetes-Related Vascular Complications: Addressing issues like diabetic retinopathy or peripheral vascular disease.
- Autoimmune Diseases: Where improved gene modulation could help regulate abnormal inflammatory responses.
Such applications underscore the importance of refining gene delivery systems, not only for their immediate therapeutic impact but also for their ability to pave the way for future research across a broad range of medical disciplines.
Addressing the Overwhelming Challenges in Vector Engineering
While the advances in modifying AAV variants are promising, the task of engineering these vectors is still loaded with problems. The laboratory work involved in tweaking the viral capsid, ensuring proper gene packaging, and verifying safety and efficacy is a delicate balancing act. Researchers must figure a path through a series of complicated pieces, each representing a potential stumbling block to clinical success.
Tackling the Hidden Complexities of Vector Design
There are many subtle parts in the design and engineering of viral vectors. Some of the most challenging areas include:
- Maintaining Structural Integrity: Ensuring that the modifications do not compromise the overall stability of the virus.
- Optimizing Capsid Chemistry: Making precise adjustments to improve cell specificity while avoiding adverse immune responses.
- Quality Control in Manufacturing: Producing high-purity viral batches that are consistent from one production run to the next.
These little details illustrate why working through every twist and turn of vector design requires not only technical expertise but also a keen understanding of cellular biology. Each adjustment must be carefully tested and validated in preclinical models, a process that can be both overwhelming and time-consuming. Yet, as researchers slowly untangle these complicated pieces, the pathway to effective and safe gene therapies becomes clearer.
Strategies to Manage Manufacturing Challenges
Another key aspect of transforming laboratory breakthroughs into clinical realities is ensuring that the manufacturing process can be scaled up without losing quality or efficacy. Some of the strategies adopted to meet this challenge include:
- Standardized Production Protocols: Adopting uniform protocols to minimize batch-to-batch variability.
- Advanced Purification Techniques: Utilizing high-precision filtration and chromatography to isolate the viral vectors.
- Rigorous Quality Assurance: Implementing multi-tiered testing processes to ensure the vector meets all necessary safety and efficacy standards.
These strategies help soothe some of the nerve-racking concerns associated with the production of large-scale viral vectors. By establishing clear guidelines and robust testing protocols, scientists and manufacturers can work together to ensure that the manufacturing process is as refined as the vectors themselves.
Looking Ahead: The Future of Modified AAV Vectors in Medicine
Despite the many challenges and tricky parts detailed above, the outlook for modified AAV vectors in gene therapy remains extremely promising. As technology continues to evolve, so too does our ability to craft precise, effective therapies that address a range of medical conditions at their very source. The work done by research groups in refining these viral vectors heralds a new era of personalized, precision medicine.
Key Areas of Future Research
Looking forward, there are several areas where further research is super important to enhance the success of gene delivery systems:
- Further Capsid Optimization: Continued exploration into the small distinctions in capsid protein structure to maximize cell-targeting efficacy.
- Long-Term Efficacy Studies: Extended research to monitor gene expression over prolonged periods, ensuring that therapeutic benefits are maintained.
- Expanding Therapeutic Applications: Investigating the potential of these vectors in other chronic and degenerative diseases beyond cardiovascular health.
- Improved Dosing Regimens: Refining the balance between efficacy and safety to further enhance clinical outcomes.
- Integrative Approaches: Combining modified viral vectors with advanced imaging and biomarker analyses to monitor in vivo performance in real time.
Collaborative Efforts and Regulatory Considerations
The path between bench research and bedside application is full of twists and turns. It is both critical and challenging to work through this process in close collaboration with regulatory bodies, ensuring that all the subtle parts of vector modification and production meet the highest safety standards. Researchers, clinicians, and regulatory experts must work together to figure a path that accelerates the journey from experimental success to widespread clinical application.
Regulatory guidelines for gene therapy have evolved considerably in recent years as the science behind these approaches has matured. The integration of improved manufacturing practices, along with robust clinical data, is key to driving regulatory approval. Moving forward, collaborative oversight will be a cornerstone of ensuring that these innovative therapies can be safely and effectively brought to patients worldwide.
Conclusion: Embracing the Future of Precision Gene Therapy
In conclusion, the evolution of modified AAV variants represents a critical leap forward in the field of gene therapy. By addressing the trickier aspects of gene delivery—such as enhancing specificity for human vascular endothelial cells and overcoming immune system barriers—researchers are paving the way for more effective and tailored therapeutic options. The study led by Stamataki et al. is a prime example of how systematic vector modifications can make a significant difference in transduction efficiency and overall treatment outcomes.
While there are still plenty of complicated pieces to work through—from ensuring long-term safety to managing manufacturing challenges—the progress made thus far is both exciting and encouraging. These advancements not only promise to improve the management of cardiovascular diseases but also open the door for treating a host of other conditions where targeted gene delivery can make a lasting impact.
As the science of gene therapy continues to mature, the integration of these improved vectors into clinical practice represents a transformative moment in modern medicine. With careful attention to the fine details and a willingness to tackle every twist and turn of the development process, the future of precision gene therapy looks brighter than ever.
Ultimately, the journey from innovative research to real-world treatment is complex and sometimes overwhelming. However, by systematically addressing each confusing bit and tangled issue through collaborative efforts, technical refinements, and ongoing clinical validation, we are steadily finding our way toward a new era of medicine—one where safe, effective, and personalized gene therapies become an everyday reality for patients around the globe.
In summary, the modified AAV vectors not only provide a promising solution to longstanding challenges in gene therapy but also highlight the importance of ongoing research and collaboration in advancing therapeutic frontiers. Whether it is by enhancing transduction efficiency in difficult-to-treat cells or by establishing new standards in vector safety and manufacturing, every development brings us one step closer to overcoming the nerve-racking obstacles that have historically limited the potential of gene-based treatments.
As we take a closer look into the future, it is clear that these refined viral vectors will play a critical role in shaping the next generation of therapies. With continued investment in research, development, and regulatory collaboration, the advancements seen today could soon translate into life-changing treatments for countless patients, fulfilling the longstanding promise of gene therapy in modern medicine.
Originally Post From https://www.geneonline.com/study-explores-modified-aav-variants-to-enhance-gene-delivery-in-human-vascular-endothelial-cells/
Read more about this topic at
Optimized AAV capsids for basal ganglia diseases show …
Development of Optimized AAV Serotype Vectors for High- …